For Healthcare Professionals:
Patients followed by the NPHVA (PNAVD) require chronic ventilatory assistance. For some patients, not using their ventilatory assistance device may lead to severe consequences such as acute hypercapnia, hypoxemia and death. For this reason, we request that you provide access to a ventilatory assistance device to patients who are using one daily. We also ask you to not administer oxygen without ventilatory support for this clientele as it may result in CO2 retention. If in doubt or if there are signs of hypercapnia, check the PCO2.
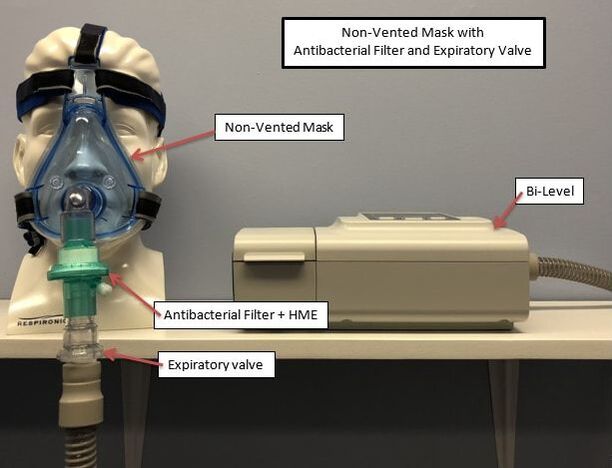
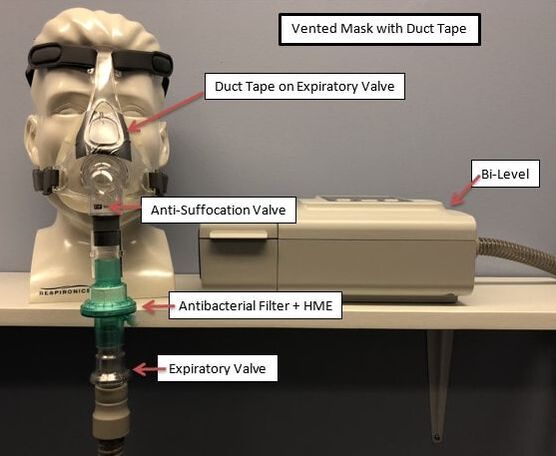
We are aware that non-invasive ventilation is an Aerosol Generating Medical Procedure (AGMP’s) and that healthcare facilities should take this into consideration. European and American studies have advocated bi-level use during hospitalization for patients using long-term home ventilation. To reduce the risk of contamination via aerosols:
Patients followed by the NPHVA (PNAVD) require chronic ventilatory assistance. For some patients, not using their ventilatory assistance device may lead to severe consequences such as acute hypercapnia, hypoxemia and death. For this reason, we request that you provide access to a ventilatory assistance device to patients who are using one daily. We also ask you to not administer oxygen without ventilatory support for this clientele as it may result in CO2 retention. If in doubt or if there are signs of hypercapnia, check the PCO2.
We are aware that non-invasive ventilation is an Aerosol Generating Medical Procedure (AGMP’s) and that healthcare facilities should take this into consideration. European and American studies have advocated bi-level use during hospitalization for patients using long-term home ventilation. To reduce the risk of contamination via aerosols:
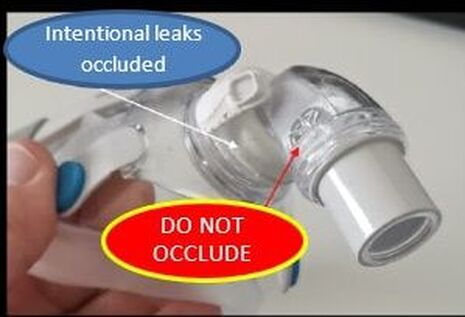
- A well-adjusted facial mask decreases aerosol dispersion. It is not recommended to use a nasal mask or pillows.
- Put the mask on before turning on the device and take it off after turning it off.
|
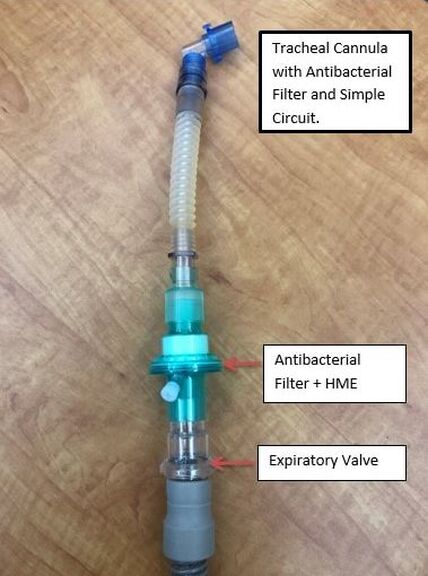
- An antibacterial filter with HME is recommended. Do not use heated humidifiers.
- Filters must be verified regularly during a 24 hour period and changed as soon as they become humid. A humid filter will be inefficient and may increase resistance.
- An oxygen connector may be inserted in the circuit between the mask and the filter.
|
Other applications in NIV:
To help during the current pandemic situation and to meet the needs for NIV, some French and American Medical Centers use:
|
WARNING: THIS METHOD SHOULD ONLY BE USED AS A LAST RESORT AND HEALTHCARE PROFESSIONALS MUST MAKE SURE THAT AN EXPIRATORY VALVE IS INSERTED IN THE CIRCUIT.
|
Patients with tracheal cannula
|
References:
AK Simonds, Evaluation of droplet dispersion during non-invasive ventilation, oxygen therapy, nebuliser treatment and chest physiotherapy in clinical practice: implications for management of pandemic influenza and other airborne, Infections Health Technology Assessment 2010; Vol. 14: No. 46, 131–172
David S. Hui, Exhaled air dispersion during high-flow nasal cannula therapy versus CPAP via different masks, European Respiratory Journal 2019 53: 1802339; DOI: 10.1183/13993003.02339-2018
http://splf.fr/gavo2/
Khai Tran, Aerosol Generating Procedures and Risk of Transmission of Acute Respiratory Infections to Healthcare Workers: A Systematic Review, April 2012 https://doi.org/10.1371/journal.pone.0035797
Guan L, Zhou L, Zhang J, et al. More awareness is needed for severe acute respiratory
syndrome coronavirus 2019 transmission through exhaled air during non-invasive respiratory support: experience from China. Eur Respir J 2020; 55: 2000352 [https://erj.ersjournals.com/content/55/3/2000352].
AK Simonds, Evaluation of droplet dispersion during non-invasive ventilation, oxygen therapy, nebuliser treatment and chest physiotherapy in clinical practice: implications for management of pandemic influenza and other airborne, Infections Health Technology Assessment 2010; Vol. 14: No. 46, 131–172
David S. Hui, Exhaled air dispersion during high-flow nasal cannula therapy versus CPAP via different masks, European Respiratory Journal 2019 53: 1802339; DOI: 10.1183/13993003.02339-2018
http://splf.fr/gavo2/
Khai Tran, Aerosol Generating Procedures and Risk of Transmission of Acute Respiratory Infections to Healthcare Workers: A Systematic Review, April 2012 https://doi.org/10.1371/journal.pone.0035797
Guan L, Zhou L, Zhang J, et al. More awareness is needed for severe acute respiratory
syndrome coronavirus 2019 transmission through exhaled air during non-invasive respiratory support: experience from China. Eur Respir J 2020; 55: 2000352 [https://erj.ersjournals.com/content/55/3/2000352].
|
Social media
|
Copyright © 2024 NPHVA All Rights Reserved.